IVF
What Is IVF?
In vitro fertilization, or IVF, is a form of assisted reproductive technology (ART). During IVF, an egg is fertilized in the lab with a single sperm. The fertilized egg is given time to mature in the lab and the resulting embryo is then transferred to the uterus of the mother or surrogate.
Who Can Benefit from IVF?
In vitro fertilization is an assisted reproductive technology recommended to patients struggling with issues such as:
- Ovulation problems
- PCOS
- Endometriosis
- Male factor infertility
- Unexplained infertility
- Fallopian tube problems
- Recurrent miscarriage
- Failed fertility treatment

Wondering If IVF Is Right for You? Call us to schedule your consultation today
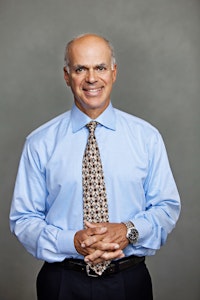
If you have struggled to have a child, it can be an immense emotional challenge. At the Center For Reproductive Medicine And Fertility in Voorhees, NJ, our fertility experts, Dr. Manara and Dr. Dougherty, are here to help guide you through the process. Our doctors have helped many patients who have been unsuccessful in previous attempts to conceive for a variety of reasons. Our highly personalized IVF cycles are customized to your unique needs to give you the best chances of a successful pregnancy.
Wondering if IVF is right for you? Take the first step by requesting a consultation. Contact us online or give us a call today:
(856) 767-0009

Patients Love The Center For Reproductive Medicine And Fertility
Dr.Manara and his staff are the best. I wish Dr. Manara would also deliver babies because I was released today and it was bittersweet. Kelly at the front desk is so warm and knowledgeable. The ultrasound tech is incredible, she is a professional at what she does ! I wouldn't hesitate to recommend or use this doctor again ! thank you!
View on GoogleDr. Louis Manara is a great doctor. He takes the time to answer all questions and concerns. He is knowledgeable, sensitive, and informative. I immediately felt at ease in his care. His staff is great, too. HIGHLY recommend to anyone looking for a specialist! Thank you Dr. Manara and to everyone in your office!
View on GoogleIn Vitro Fertilization Treatment Timeline
Have questions about the IVF timeline?
What Is the Success Rate of IVF?
Advancements in assisted reproductive technology mean more people than ever can achieve their dreams of a successful pregnancy. However, your chances of success depend on a number of factors, including your age, your health, the cause of infertility, previous pregnancies, and more. The CDC has developed a success rate estimator that can give you an idea of your chances of conception using IVF.
Ready to Begin Your IVF Journey? Call us today to get started
Dr. Manara, Dr. Dougherty, and our team of fertility experts thrive on the success stories of our patients. At our fertility clinic in Voorhees, NJ, we provide individualized treatment and use advanced solutions to help patients conceive. Our treatment plans are intended not only to identify infertility issues, but also to effectively treat them so our patients can experience the joys of a family.
The Center For Reproductive Medicine and Fertility has been providing a high level of care for hopeful parents since 1985. We are able to personalize patient care in a friendly, caring environment. We try our very best to provide the support, education, and kindness needed to get through this process. We strive to get to know our patients as individuals so that we can individualize the care we provide.
Request a consultation by contacting us online or calling our Voorhees, New Jersey, fertility clinic to begin your IVF journey today.
(856) 767-0009
Patients Recommend Our Voorhees, New Jersey, Practice
My wife and I had trouble getting and staying pregnant. We had been through two other doctors before a friend recommended Dr. Manara. Now, we are expecting twins—and we didn’t even have to go through IVF at this practice. The results speak for themselves.
View on GoogleDr. Manara is super compassionate and knowledgeable in his field. I’m glad that friends recommended him for our fertility journey! The front desk staff is the friendliest I’ve ever seen in a doctors office. They make you feel comfortable all around!
View on GoogleEgg Retrieval Facts
- Before the procedure begins at our New Jersey fertility clinic, you will be given a mild sedative by our licensed nurse anesthetists (CRNAs), and your vitals are monitored throughout the procedure.
- Using intra-vaginal ultrasound to guide him, your doctor will pass a needle through the vaginal wall and into the ovary to complete the egg retrieval. Each of the follicles containing the eggs may be aspirated using gentle, carefully monitored suction.
- The entire egg removal procedure takes approximately 15 minutes. You will be monitored for about an hour as the medication wears off.
- You will then be discharged to rest at home. Most patients return to normal activities the following day. Using traditional methods or intracytoplasmic sperm injection (ICSI), your eggs will be fertilized and monitored for growth.

In Vitro Fertilization Glossary
Fallopian Tubes
Fallopian tubes are the tubes that connect the ovaries to the uterus. The fallopian tubes allow the egg to travel from the ovaries to the uterus.
ICSI
ICSI is short for intracytoplasmic sperm injection, the process of directly injecting a healthy sperm into the egg.
Embryo
The embryonic stage is the first stage of development of a fertilized egg. A healthy embryo is transferred during the IVF cycle where, if successful, it will implant into the mother or surrogate's uterus.
Implantation
The process in which an embryo implants into the uterus during the earliest stages of pregnancy.
More Praise for Our Voorhees, NJ, Fertility Clinic
I cant say enough good things about Dr Manara and his staff! I went in for pcos related infertility after trying for years with no luck. I can happily say thanks to Dr Manara and staff I just had my last appointment with them at 8 weeks pregnant!! The staff is very attentive and come across as actually caring about you not just rushing you in and out. I could call them with any questions and concerns and they got me answers quickly! I will recommend them to anyone I know looking for an infertility doctor!
View on GoogleSo fortunate after a year of trying to conceive our second child we sought the help of Dr. Manara. Dr. Manara always had time for us made us feel very comfortable was very personable empathetic And supportive throughout the whole process. Our beautiful second daughter Stella Was just six months last week and we are truly blessed and grateful for all the help of Dr. Manara and his wonderful staff.... I Would highly recommend anyone having thoughts about a fertility specialist, Dr. Manara would be the first office I reached out to. Thank you again!!
View on Google